News - Wed, 03/14/2018 - 10:05
Colon resection
Last update 09/27/2024 - 17:58
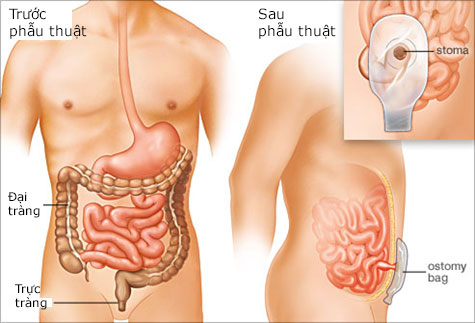
Anatomy
The colon is the part of the intestine called the "large intestine" and which comes after the small intestine. The first portion of the colon is located on the right side (ascending colon) then the colon goes through the abdomen from the right to the left (transverse colon), descends down to the left part of the abdomen (left colon) before ending with a colonic loop (colon sigmoid) which continues into the terminal portion of the large intestine, the rectum.
When is colon resection done?
Colon resection or colectomy is applied to treat several benign (polyps, sigmoid diverticulitis) as well as malignant conditions (cancers). The risks involved are related to the content of the large intestine, which are basically feces and therefore septic and to a lesser extent disorders related to the blood vessels supplying the large intestine which may lead to a larger surgery than expected. There are several types of colectomies: right, left, sigmoid, transverse and possibly total, depending on the underlying condition and the extent of lesions to be removed.
After resection of the diseased part of the large intestine, the two ends need to be reconnected. This is called an anastomosis and can be done either manually by suturing the ends together or by utilizing a mechanical stapler. The anastomosis is named after the parts of the large intestine which are connected together: ileo-colic, colo-colic or colo-rectal anastomosis.
If there are problems with the lower part of the large intestine an ileostomy or colostomy may be necessary to temporarily divert stool out of the colon. A stomy is a surgical procedure that brings one end of the large intestine out through the abdominal wall. During this procedure, one end of the colon is diverted through an incision in the abdominal wall to create a stoma, which is practically an artificial anus. A stoma is the opening in the skin where a pouch for collecting feces is attached.
This may be necessary, especially during an intervention carried out in emergency (occlusion, or peritonitis with perforation), or for anastomosis with a higher risk of fistula.
What types of surgeries are available?
This intervention can be done either by laparoscopic or open surgery. Laparoscopic or ‘key hole’ surgery is a minimally invasive technique which allows the surgeon to perform many common colon procedures through small incisions. In most laparoscopic colon resections surgeons operate through 4 or 5 small holes (each a couple of centimeters). Through these holes, instruments are inserted into the belly and the surgeon can watch an enlarged image of the patient’s internal organ on a video screen. Sometimes the incisions need to be slightly enlarged. The advantage of this technique is less scarring and postoperative pain and faster healing. Depending on the procedure patients may leave the hospital after a few days and return to normal activities more quickly than with open surgery. In case of difficulties, the surgeon may have to stop the laparoscopy and proceed with a classic open surgery (conversion to laparotomy). In this case the abdominal incision will usually be located in the middle of the abdomen; it can sometimes be in the fold of the waist.
What are the possible complications?
No surgery comes without some risks. Risks, however are very rare and generally well controlled. Your surgeon will discuss with you in detail the risks and benefits of each treatment option for you to decide together which procedure is the best suitable for your condition.
Complications during the procedure:
- Injury of viscera near the surgical site: digestive (intestine) or urinary (ureter, bladder) may rarely be injured accidentally if a procedure is very complex or if the patient has some unforeseen anatomy. Their immediate recognition generally allows a repair without sequela. In rare cases a temporary stoma or insertion of a ureteral probe may be necessary.
- Hemorrhage: bleeding can occur, which is usually quickly controlled, but may require a transfusion of blood or blood products. Due to strict controls of the donor blood complications from transfusions, such as infectious disease transmission has become exceedingly rare.
- Nerve compression: the surgical team must be attentive to the positioning of the limbs to avoid any compression of nerves or the soft tissue during the intervention. If a nerve compression occurs, it generally disappears by itself within a few weeks. It is extremely rare that a patient shows persistent numbness or a tingling sensation over the skin of the affected limb/area. Equally seldom are injuries to the skin due to the application of skin disinfectants, electrode stickers and electric current.
Postoperative complications
Follow up after surgery in the majority of cases is simple. Patients can start oral feeding usually after 2-3 days and can leave the hospital approximately after 1 week. Complications are rare, the most common ones are:
- Anastomotic fistula (around 5%): usually occurs around the 4-5th day after surgery. If the anastomosis does not heal properly there is a risk to develop an abscess and peritonitis (inflammation of the lining of the bowel). This may require a drainage, re-intervention, and creation of a temporary stoma and will increase duration of in-hospital stay.
- Bleeding: an anastomosis can be responsible for secondary bleeding or hematoma that may require re-intervention and/or a transfusion.
- Infections: despite aseptic precautions and antibiotic therapy, surgical site infections can occur. They are most commonly treated by simple evacuation, and careful changing and monitoring of the bandages until healed.
- Bowel obstruction: can occur after any abdominal intervention and may require the installation of a prolonged naso-gastric probe and/or re-intervention. It may happen if the intestine twists around itself.
General complications
Phlebitis, or pulmonary embolism, these complications are rare due to systematic prevention which is carried out by a preventive anticoagulant treatment and the use of compression stockings.
Ask your surgeon to discuss all available options in detail with you.
This information is for education purposes and is not intended to replace a consultation with specialist doctor. For further information about appendicitis, please contact us at: (84-24) 3577 1100 or send us an inquiry here